Dipping Your Toes in Sobriety: Is "Dry January" Safe for Heavy Drinkers?
As the holiday season winds down and the confetti from New Year's Eve is swept away, millions of Americans turn their attention to resolutions. In recent years, one public health trend has dominated the conversation: Dry January.
The challenge is simple in theory: stop drinking alcohol for the entire first month of the year to reset your body and mind. For the casual "social drinker" who overindulged during the holidays, this challenge is a fantastic way to detox and save some money.
However, at More Than Rehab, we see a different side of this trend. For those with a physical dependency on alcohol, deciding to suddenly stop drinking alcohol cold turkey on January 1st isn't just difficult - it can be deadly. If you are considering cutting out alcohol this year, it is vital to understand the difference between a healthy "reset" and a dangerous medical crisis.

The Appeal: Benefits of Dry January
It’s easy to see why this challenge has gone viral. Even taking a month off from drinking can have profound effects on the body. Public health campaigns often highlight the benefits of Dry January week by week, which can be incredibly motivating for the average person.
- Week 1: Better sleep quality and increased hydration.
- Week 2: Acid reflux symptoms often decrease, and you may notice clearer skin.
- Week 3: Blood pressure levels may begin to lower, and many report weight loss.
- Week 4: The liver begins to heal (reducing liver fat), and the immune system gets a significant boost.
Beyond the physical, participants often report long term mental health benefits, such as reduced anxiety and a clearer head. For someone whose drinking is purely habitual, these wins are a great reason to limit alcohol consumption or take a break.
When the Resolution Becomes Dangerous
While the benefits of dry January are real, they come with a massive asterisk. Alcohol is one of the few substances where withdrawal can be fatal.
If you are a heavy, daily drinker, your brain has adjusted its chemistry to function with alcohol present. Alcohol is a depressant, so your brain produces extra stimulating chemicals to counteract it. When you abruptly remove the alcohol (like waking up on January 1st and swearing off the bottle) those stimulating chemicals flood your system unchecked.
This is why we urge caution. If you find yourself physically needing a drink to start the day, to stop the shaking, or to feel "normal," cutting out alcohol without medical supervision is very risky.
Is Cold Turkey Dangerous for Alcoholics?
The short answer is yes. For dependent drinkers, the "cold turkey" approach can shock the central nervous system.

Alcohol withdrawal symptoms can start as soon as 6 hours after your last drink. At first, they might feel like a bad hangover or the flu, including:
- Anxiety and irritability
- Insomnia
- Nausea and vomiting
- Tremors (the "shakes")
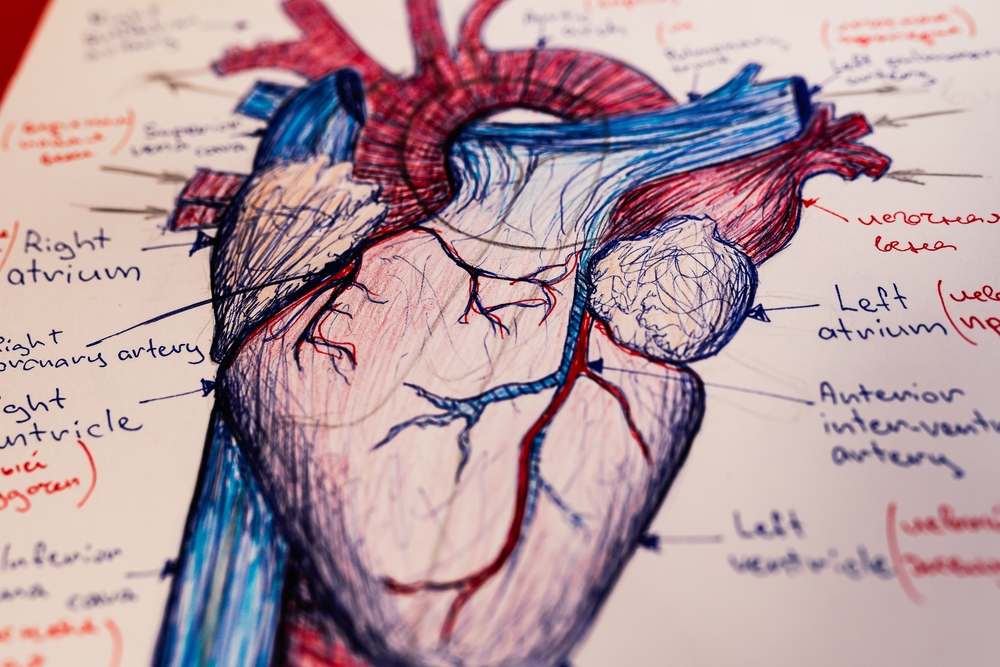
- Sweating and elevated heart rate
However, for severe alcoholics, these symptoms can escalate quickly into a life-threatening condition known as Delirium Tremens (DTs). DTs can cause severe confusion, hallucinations, dangerous spikes in blood pressure, and grand mal seizures. Without immediate medical intervention, these seizures can be fatal.
The "Dry January" Test
We often tell clients that trying Dry January is actually a fantastic diagnostic tool. If you decide to stay sober for the month and you find it annoying but manageable, you likely don't have a severe physical dependency.
But, if you decide to stop and you experience physical alcohol withdrawal symptoms, or if the mental craving is so intense that you are white-knuckling it by January 3rd, that is your sign. It means your relationship with alcohol has crossed the line from a behavioral pattern into a physical dependence.
If you fail at Dry January, do not beat yourself up. It doesn't mean you are weak; it means you might have an alcohol use disorder (AUD). And just like any other illness, you need professional treatment options, not just willpower.
Safe Sobriety: Medical Detox for Alcohol Texas
If you suspect you are physically dependent on alcohol, please do not attempt to detox on your couch. The safest way to begin your recovery journey is through a full medical detox for alcohol Texas program, like the one we offer at More Than Rehab.
Medical detox provides a safe, monitored environment where medical professionals can administer medications to ease withdrawal symptoms and prevent seizures. We monitor your vitals, including your blood pressure, 24/7 to ensure you are safe.
Once the alcohol is safely out of your system, you can truly begin to experience the mental clarity and immune system recovery that Dry January promises - but you will be doing it with a safety net.

Beyond January: A Life of Recovery
Dry January is a catchy slogan, but recovery is a lifestyle. Whether you are looking to limit alcohol consumption or quit entirely, understanding your own biology is the first step.
At More Than Rehab, we believe in the social model of recovery. We know that isolation feeds addiction, which is why attempting a "solo" Dry January often fails for those who need it most. We offer a community that supports you not just for a month, but for a lifetime.
If you are ready to make a change this New Year, do it safely. Don't gamble with your health.
Frequently Asked Questions
Q: Can I do Dry January if I drink every day?
A: If you are a heavy daily drinker, you should consult a doctor before stopping abruptly. Sudden cessation can trigger severe alcohol withdrawal symptoms. It is often safer to taper off or enter a medical detox for alcohol at a trusted Texas facility to ensure your safety.
Q: What are the first signs of dangerous alcohol withdrawal?
A: Beyond standard hangover symptoms, watch for severe tremors (shaking hands), hallucinations (seeing or hearing things that aren't there), confusion, and a racing heart. These are signs of delirium tremens and require immediate emergency medical attention.
Q: What are the long-term benefits of quitting alcohol?
A: Cutting out alcohol long-term significantly reduces your risk of liver disease, heart disease, and certain cancers. It also boosts your immune system, lowers blood pressure, and provides substantial long term mental health benefits like improved mood stability and memory.
Q: What treatment options are available if I can't stop on my own?
A: If willpower isn't enough, treatment options range from outpatient therapy and support groups to inpatient rehabilitation. At More Than Rehab, we offer a full continuum of care, starting with medical detox and moving into therapy and social support to help you stay sober.
Make this New Year the one that changes everything. If you are worried about your drinking or withdrawal symptoms, call More Than Rehab today at 888-249-2191. We are here to help you detox safely and start fresh.