The Deadliest Night of the Year: Why New Year's Eve Spells Disaster for Routine Users
For most of the world, New Year’s Eve is a time of celebration, fireworks, and looking forward to a fresh start. But for those of us in the recovery community, and for those still actively struggling with substance use, we know it by a different name: "Amateur Night."
It is the one night of the year when the entire world decides to party to excess. Friends or family who usually have a single glass of wine are suddenly doing multiple shots. The bars are packed shoulder-to-shoulder, and the streets are flooded with erratic drivers.
For someone currently battling addiction, NYE celebrations aren't just a party; they are a minefield. The pressure to "go big" often leads to risky behaviors that can end in tragedy. At More Than Rehab, we want to be blunt about the reality of the streets on December 31st. The drug supply is more toxic than ever, the roads are heavily policed, and the risks of mixing alcohol and cocaine or other substances are at an all-time high.
If you are thinking about going out this year, we urge you to reconsider. Here is why staying alcohol free and safe at home might be the best decision you'll ever make.

The Supply Chain is Toxic: Fentanyl in Party Drugs
The most terrifying aspect of the modern drug landscape is the utter lack of quality control. On New Year's Eve, demand for illicit substances skyrockets. To meet this demand, dealers often "stomp on" (dilute) their supply to stretch it further, or they clear out their old, low-quality inventory on unsuspecting "holiday partiers."
In recent years, we have seen a massive spike in fentanyl in party drugs. It is no longer just heroin users who need to be afraid. Fentanyl is being pressed into fake prescription pills (like Xanax, or Adderall) and cut into cocaine and MDMA (ecstasy, or "molly"). As we have noted before, even "innocent" looking powders can be deadly; cocaine is frequently cut with fentanyl, a powerful opioid that can be fatal even in very small amounts.
On a night like New Year's Eve, when judgment is impaired and consumption is high, you simply cannot trust what you are buying. You are not just rolling the dice on a "good time"; you could be rolling the dice on your life.
The Danger of Polysubstance Abuse
Another major risk on New Year's Eve is the tendency to mix substances. You might start with a few drinks, then someone offers you something else to "wake up" or "keep the party going."
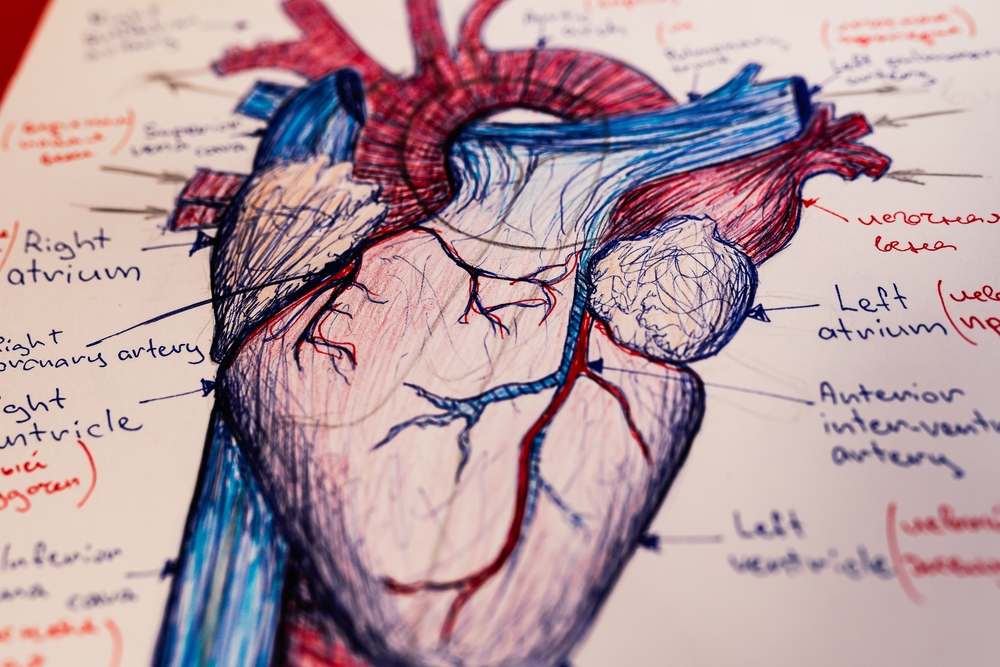
The risks of mixing alcohol and cocaine are particularly severe. Many people combine these to counteract the drowsiness of alcohol, but this combination creates a unique chemical in the liver called cocaethylene. This compound is far more toxic to the heart than either drug alone and significantly increases the risk of sudden cardiac arrest.
Furthermore, mixing depressants (like alcohol) with stimulants masks the effects of the alcohol, leading you to drink far more than your body can handle, which can result in accidental overdose and death.

The same applies to other combinations common at bar crawls or house parties. Mixing alcohol with MDMA (Ecstasy/Molly) can lead to severe dehydration and overheating , while mixing alcohol with prescription opioids or benzodiazepines can cause your respiratory system to shut down completely.
NYE DUI Checkpoints Texas: The Law is Watching
If the health risks aren't enough to make you pause, the legal ones should be. New Year's Eve is the "Super Bowl" for law enforcement. Police departments across Texas step up their patrols, and NYE DUI checkpoints Texas becomes a top trending search term for a reason.
Officers are on high alert for any sign of impairment. Even if you think you are a "safe" driver or have a high tolerance, the chaos of the night works against you. Other drivers are unpredictable, and a minor fender bender caused by someone else can turn into a life-altering felony for you if you have drugs or alcohol in your system, or in your possession.
Is one night of partying worth a permanent criminal record, thousands of dollars in legal fees, or the guilt of injuring another innocent person?
Why "Designated Drivers" Aren't Always Enough
We often hear the advice to just get a designated driver or use a rideshare app. While this keeps you from driving, it doesn't protect you from the other dangers of the night.
- Social Friction: Being the most intoxicated person in a rideshare or at a party leaves you vulnerable to theft, assault, or arrest.
- Triggering Environments: For someone trying to cut back or quit, being surrounded by binge drinking and drug use is incredibly triggering. It reinforces the cycle of addiction.
- The "Amateur" Factor: Arguments and bar fights are statistically more common on NYE. Being in that environment puts you in physical danger, even if you aren't the one starting the trouble.
How to Ring in the New Year Safely
The safest way to survive New Year's Eve is to opt out of the madness entirely. We know the Fear Of Missing Out (FOMO) is real, but waking up on January 1st without a hangover, a court date, or a hospital bill is a feeling that beats any party.
Here is how to have a fulfilling, alcohol free night:
- Host a Sober Gathering: Invite friends or family members who are supportive of your sobriety. Board games, movies, and good food create connection without the chemical haze.
- Reflect and Reset: Use the evening to journal or meditate on your goals. If you are in addiction recovery, reflect on how far you have come in the past year.
- Stay off the Roads: If you don't have to go out, don't. The roads are dangerous on NYE, regardless of your own sobriety.
- Connect with Your Support Group: Many recovery groups host "Alkathons" or sober New Year's Eve party events. These are safe havens filled with people who understand exactly what you are going through.
Glad You Stayed Sober? Keep It Going.

If you wake up on January 1st feeling clear-headed and healthy, hold onto that feeling. It is a stark contrast to the shame and sickness that usually follows a NYE bender.
However, if you find that you couldn't stay sober, or if the holidays have highlighted a dependency you can no longer ignore, More Than Rehab is always here to help you. We understand the unique pressures of the holiday season and the grip of fentanyl in party drugs and other substances.
We offer comprehensive addiction treatment programs, including medical detox and dual diagnosis care, to help you break the cycle. You don't have to wait for a resolution to change your life.
Frequently Asked Questions
Q: Are overdose rates really higher on New Year's Eve?
A: Yes. New Year's Eve overdose statistics consistently show a spike in drug and alcohol-related emergencies. The combination of binge drinking, the prevalence of adulterated drugs (like fentanyl), and the "amateur" nature of the holiday creates a perfect storm for medical crises.
Q: I suspect my family member is using drugs. Should I confront them on NYE?
A: It is generally unsafe to confront someone while they are intoxicated or under the influence, especially in a high-stress environment like a New Year's Eve party. It is better to ensure their immediate physical safety (like taking their keys) and wait until they are sober to have a conversation about addiction treatment.
Q: What makes mixing alcohol and cocaine so dangerous?
A: Mixing alcohol with cocaine creates cocaethylene in the liver, which is highly toxic to the heart. Additionally, cocaine is a stimulant that masks the depressant effects of alcohol, leading users to drink dangerous amounts of alcohol without realizing they are approaching alcohol poisoning.
Q: How can I find a sober event for New Year's Eve in Texas?
A: Many local AA/NA chapters and community centers host alcohol-free "Alkathons" or parties. A quick search for "sober NYE events near me" or contacting a local addiction treatment center for recommendations is a great way to find a safe community to ring in the new year safely.
Do not let one night of partying cost you your future. If you are struggling with substance abuse, call More Than Rehab today. We are available 24/7 to help you start your journey to recovery.