Winter Blues or Relapse Warning? Navigating Seasonal Depression in Recovery
The holidays are over. The decorations are packed away, the family has gone home, and the "New Year, New Me" excitement is starting to wear off. Now, we are left with the gray skies, cold winds, and short days of January and February that for many, lead to the "winter blues".
For many people in recovery, this specific time of the year is dangerous. You might feel heavy, unmotivated, or irritable. You might tell yourself, "I'm just having a bad week," but if these feelings persist, you might be dealing with seasonal affective disorder (SAD).
Understanding the link between SAD and addiction is vital because, for us, "winter blues" aren't just annoying—they are a direct relapse trigger. If left unchecked, this condition can jeopardize your sobriety, making it crucial to recognize the signs and have a solid plan in place.
What is Seasonal Affective Disorder?
Many people joke about the "winter blues," but seasonal affective disorder is a clinically recognized condition. It is a specific type of depression that follows a seasonal pattern, typically starting in late fall and peaking in January and February.

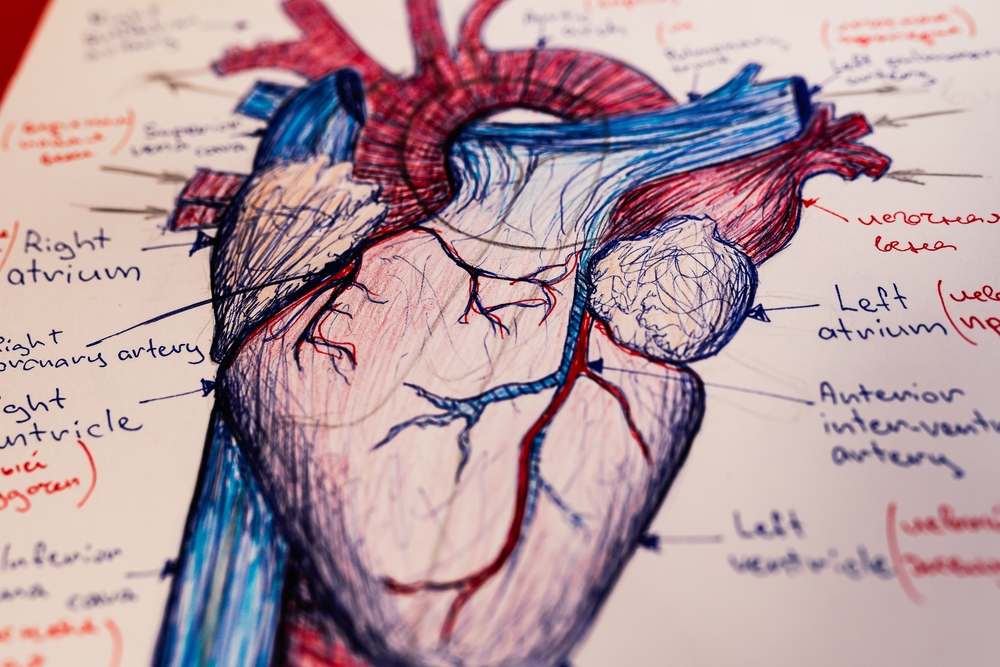
It is not just about "being sad about the weather." It is a biological response to a lack of sunlight, which disrupts your body’s circadian rhythm and serotonin levels. Unlike typical depression, which might cause insomnia or a loss of appetite, SAD often presents itself with unique symptoms that can feel physical:
- Weight Gain: A craving for carbohydrates and comfort foods is common, leading to noticeable weight changes.
- Disrupted Sleep Patterns: Instead of insomnia, you might find yourself oversleeping (hypersomnia) but still waking up exhausted.
- Heavy Limbs: A physical sensation of your arms and legs feeling "heavy" or weighed down.
- Social Withdrawal: The urge to "hibernate" and isolate from friends and support networks.
The Addiction Connection: Why We "Self-Medicate"
For someone with a history of drug addiction or alcoholism, these symptoms are terrifyingly familiar. The lethargy and low mood caused by SAD can feel exactly like the onset of withdrawal or deep depression.
When your brain is low on serotonin (the "feel-good" chemical), it starts looking for a quick fix. In the past, that fix was substances. This is where the danger lies: people often begin self-medicating to combat the winter gloom without realizing they are battling a chemical imbalance caused by the season.
You might think, "I'm sober, so why do I feel this miserable?" That thought process is a trap. It leads to the lie that drugs or alcohol were the only things that made you feel "normal." Recognizing that your mental health is being affected by the season—not a failure of your program—is the first step in staying safe.
Dual Diagnosis Seasonal Affective Disorder
At More Than Rehab, we treat addiction as a dual diagnosis issue. This means we don't just look at the substance abuse; we look at the underlying mental health conditions driving it.
Dual diagnosis with seasonal affective disorder is more common than you might think. Studies suggest that people with SAD are significantly more likely to struggle with substance abuse than the general population. If you treat the addiction but ignore the seasonal depression, you are leaving a back door open for relapse.
Effective treatment requires addressing both. You cannot simply "white knuckle" your way through seasonal depression. Just as you wouldn't ignore a broken leg, you shouldn't ignore a brain chemistry imbalance just because the calendar says it's January.

Building Your Winter Sobriety Tips & Action Plan
Surviving the winter slump requires more than just willpower; it requires strategy. Here are some practical winter sobriety tips to help you stay on track.
1. Update Your Relapse Prevention Plan
A relapse prevention plan is a living document. What worked for you in July might not work in January. Sit down with your sponsor or therapist and specifically map out how you will handle the next two months.
- Trigger: Dark evenings alone.
- Action: Commit to a 7:00 PM meeting or a gym class.
- Trigger: Feeling sluggish and depressed.
- Action: Schedule a doctor's appointment to check Vitamin D levels.
2. Prioritize Light and Movement
Since SAD is triggered by a lack of light, fight back with lumens. Light therapy (using a 10,000 lux lamp) is a proven treatment for this type of depression. Even 20 minutes a day can trick your brain into producing more serotonin.
Additionally, regulate your sleep patterns by waking up at the same time every day, even if it’s dark. Exercise is also non-negotiable, as it releases natural endorphins that combat the lethargy associated with addiction and winter blues.
3. Lean Into the Social Model
SAD makes you want to isolate. It tells you to stay in bed, cancel plans, and avoid people. In our social model of addiction recovery, we know that isolation is the enemy. You have to move a muscle to change a thought. Go to meetings. Stay late for coffee. If you are struggling with weight gain or fatigue, talk about it. You will likely find half the room is feeling the exact same way.

Frequently Asked Questions
Q: Can Vitamin D help with SAD and cravings?
A: Vitamin D deficiency is incredibly common in the winter and mimics symptoms of depression. While it won't stop addiction cravings instantly, correcting a deficiency can drastically improve your overall mental health and resilience against triggers.
Q: Is SAD really different from regular depression?
A: Yes. The key difference is the timing. If your depression consistently appears in late fall and resolves in the spring, it is classified as Major Depressive Disorder with Seasonal Pattern. This distinction matters because treatments like light therapy are specifically effective for this type of depression.
Q: How do I know if I'm self-medicating or just enjoying the holidays?
A: If you are using a substance (or even food/behavior) to change the way you feel because you can't tolerate your natural emotions, you are self-medicating. In recovery, we learn to sit with discomfort rather than numbing it.
Q: Should I change my recovery meetings in the winter?
A: It might be a good idea. If you usually go to evening meetings but find the dark drives depressing, try switching to a noon meeting or a morning group. Adapting your schedule to support your mental health is a smart move.
Are you or a loved one struggling to navigate the winter months sober? Don't let the season dictate your recovery. If you suspect dual diagnosis seasonal affective disorder is impacting your life, reach out for professional help.
Call More Than Rehab 24/7: