How Nitrous Oxide (Whippets) Became a Fixture at Music Festivals
Nitrous oxide (N₂O), commonly known as laughing gas, has a long history as both a medical anesthetic and a party drug. In 1799, English chemist Humphry Davy famously hosted “laughing gas” soirees, where aristocrats inhaled N₂O for its euphoric, giggly buzz. For more than 200 years, it’s been used in dentistry and medicine, often with oxygen, to safely relieve pain.
But today, nitrous oxide has taken on a new life at concerts and music festivals. Young people inhale it from whipped-cream canisters (“whippits”) or balloons for a brief high, and many assume it’s harmless. In reality, the party drug reputation hides its serious health risks.
By the latest estimates, nitrous oxide has become one of the most popular party drugs among teens and young adults. A Home Office survey in the UK found that 350,000 young people used “hippie crack,” aka: laughing gas, in one year. Annual figures on drug misuse show that 6% of all 16 to 24-year-olds had tried it. This makes it the most popular drug among teens and young adults, after cannabis.
The gas is cheap and legal to possess, and it produces uncontrollable laughter and light hallucinations. These facts have turned N₂O into a festival staple. Discarded nitrous balloons and empty canisters litter music festival fields – a scene all too common.

A Quick High: Euphoria and Dissociation
When inhaled, nitrous oxide causes an immediate, short-lived high. Users report a head-rush of euphoria, tingling sensations, light-headedness, and a fit of giggles. (This is why it’s called laughing gas.) Like a mini-anesthetic, N₂O disrupts brain neurotransmitters for a few seconds to a minute, producing dizziness, auditory and visual distortions, and a feeling of floating outside one’s body.
The high is that brief, which explains why many festivalgoers cycle through one balloon after another. Users may inhale directly from a whipped cream canister or fill a balloon or mask. Many prefer balloons so they can continue breathing air between shots of gas.
Medical experts warn that while nitrous oxide feels easy and playful at first, it can quickly cause serious acute effects. Inhaling pure nitrous oxide displaces oxygen in the lungs, so a person can easily suffocate if they pass out. “If somebody straps on nitrous oxide with a mask and loses consciousness, their oxygen level isn’t being monitored,” explains an LA County health official, “and they’re breathing N₂O, and now they’re anesthetized. People can die from suffocation”.
Frequent Use and Cumulative Harms
Nitrous oxide may look like an easy addition to a live-music vibe, but its effects on the nervous system snowball quickly. Because the high is so short-lived, many young adults keep taking balloon after balloon, and that’s where the real damage starts.

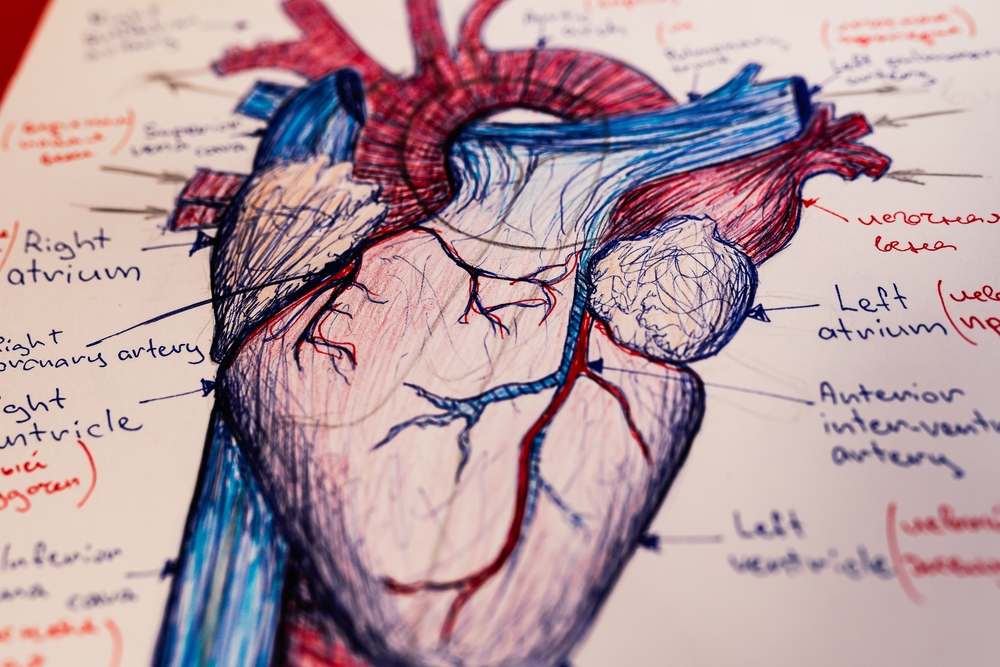
Vitamin B12 Crash → Nerve & Spinal Injury
Every inhale oxidizes vitamin B12, spikes methylmalonic acid, and starves nerves of a critical co-factor. Over weeks or months, users can slip into subacute combined degeneration: numb hands and feet, wobbly gait, brain fog, and, in severe cases, paralysis. Extra B12 won’t fix it while the gas keeps flowing; the only remedy is to stop using hippie crack altogether.
Hypoxia & Cardiovascular Stress
Pure N₂O pushes oxygen out of the lungs. Repeated hits can lead to hypoxia, seizures, irregular (tachycardic) heartbeat, and even deep-vein thrombosis. In other words, a few minutes of “laughing gas” can strain the heart and brain long after the music fades.
Freeze Burns, Aspiration & Sudden Death
Dragging gas straight from a whipped-cream charger can drop temperatures low enough to freeze airway tissue. Add alcohol or opioids, and the risk of vomiting (and then inhaling that vomit) rises sharply, a lethal combo that EMTs at Phish concerts know too well.
Mental-Health Fallout
Chronic use can amplify anxiety, depression, and dissociation, which are issues many festivalgoers already battle. When fun begins to start to feel like self-medication, that’s a red flag for escalating substance abuse.
Festivals, “Whipped-Cream” Canisters and the Nitrous Mafia
The music-festival setting uniquely encourages nitrous use and even overlooks it. Many concert organizers ban aerosol sprays and mask kits, but dealers still smuggle in bags of charged canisters. Journalists have dubbed the syndicates running festival nitrous supply “the Nitrous Mafia”. In one report, undercover buyers witnessed organized dealers selling dozens of balloons per minute outside concerts.
At multi-day campsites (like jam-band or EDM festivals), these crews might burn through hundreds of tanks, filling up to 350 balloons from each steel cylinder. For customers, it’s dirt cheap: one tank yields many 5 or 10-dollar balloons that go fast in a long set. But after a festival, security guards find balloons littered like spent bullet shells across campsites every dawn. The scene signals how deeply nitrous is woven into the current music festival culture.
Many fans have fond memories of the “old days” when someone would casually pass around a baloon as part of a communal vibe. But heavier commercialization means the drug is no longer a mellow pastime; it’s now pushed aggressively. Some musicians and crew openly complain that nitrous sales are out of control at shows.

Festivals also provide peer pressure and cues that normalize nitrous use. Among young audiences, pulling out a whipped-cream canister or balloons is almost a rite of passage. Social media amplifies this: TikTok videos and influencers often show “galaxy gas” or colored whippets as fun tricks or life hacks. Some big-name artists even glamorize it.
Rapper Kanye West publicly joked about using nitrous oxide to relieve stress. Another rapper (Lil Uzi Vert) rapped about being on “that NOS” (a slang term) on stage. These public figures make it look common and low-risk, but health experts worry this glamorization conceals the hidden harm.
Warning Signs and What Parents Should Watch For
Here’s what parents and guardians should watch for:
| What to Look For | Why It Matters |
| Balloons & whipped-cream chargers tucked into backpacks, glove boxes, or bedroom drawers | A clear sign of nitrous access—dealers known as the nitrous mafia sell these for quick, short-lived highs |
| Dizzy or giggly spells after parties or live music events | Sudden euphoria followed by confusion is classic nitrous exposure |
| Sweet or metallic breath odor | Inhaling N₂O leaves a telltale scent on clothes and skin |
| Dilated pupils, wobbling gait, numb or tingling hands/feet | Early nerve stress from rising methylmalonic acid and looming vitamin B12 deficiency |
| Headaches, chest tightness, mood swings, or new anxiety/depression | Oxygen depletion + B12 loss can damage the nervous system and overall mental health |
From Party Drug to Public-Health Alarm
What started as a quirky balloon hit at music festivals is now a fast-moving public health issue across the United States. As alcohol and pills lose their shine for some young adults, “legal highs” like nitrous oxide, ketamine, and psychedelics are filling the gap, reinforced by nitrous mafia on every concert's shakedown street. Because N₂O is still legal for culinary “whipped-cream” use, smoke shops and online stores make it look safe, yet poison-control data show nitrous-related ER visits are on the rise.
No matter how harmless “hippie crack” seems in the glow of live-music lights, every refill edges closer to real substance abuse. If you, or someone you love, has crossed that line, More Than Rehab (MTR) is here to help with evidence-based inhalant and polysubstance abuse treatment. Reach out today, before a few balloons become a lifelong battle.