Understanding Fentanyl: Why It’s So Dangerous & How to Stay Safe
The growing reports of opioid overdose deaths are overwhelming. And the rising numbers don’t make it any easier. If you’re feeling worried—about yourself, your family, or someone close to you—you’re not alone. According to the CDC, fentanyl is now involved in about 76% of opioid overdose deaths in the United States, a statistic that underscores just how serious this crisis has become.
What makes it even more frightening is how often fentanyl is mixed into other drugs without anyone realizing it. It’s understandable to feel concerned, even helpless, in the face of these risks. But understanding fentanyl, its dangers, and how to stay safe can help you take meaningful steps to protect yourself and those you care about.
What Is Fentanyl?
Fentanyl is a synthetic opioid that can be up to 50 times stronger than heroin. Doctors sometimes prescribe it to treat severe pain, especially after surgery. It is often used in hospitals under close supervision. However, fentanyl is now found more often in illegal drug markets. People sometimes buy what they believe to be prescription opioids or other drugs, only to end up with substances laced with fentanyl.
When misused or without medical supervision, fentanyl can be very harmful. Because it is so powerful, even a minimal amount can be life-threatening. This risk becomes worse when fentanyl gets mixed with other substances like cocaine or ecstasy. Sometimes, people do not even know they are taking fentanyl. That is one reason authorities are saying "one pill can kill" as so many recent overdose deaths have been attributed to unexpected fentanyl contamination in other drugs.

Why Is Fentanyl So Dangerous?
The main danger lies in its strength. Small doses can slow your breathing so much that your body shuts down, leading to an opioid overdose. This can happen before you even realize you are in trouble. When fentanyl is mixed with other drugs, it becomes even more unpredictable. People might think they are taking one substance but receive a much stronger opioid.
This often leads to a dangerous situation where just one pill or one dose can be enough to cause an overdose. As a result, the number of deaths from fentanyl overdoses continues to grow. Public health experts warn that using any non-prescribed pill is now a high-risk activity, especially if it might contain fentanyl.
How Fentanyl Can Appear in Other Drugs
Part of the reason fentanyl is dangerous is its invisibility. You can’t see, smell, or taste it, which means you cannot know if it’s there without testing the drug.
Drug dealers and drug cartels frequently lace substances with fentanyl because it’s inexpensive to produce and dramatically increases the potency of their products. This practice puts unsuspecting users at extreme risk. Fentanyl has been found in pills disguised as prescription opioids like oxycodone, in fake pills made to look like medications, and even mixed with drugs like cocaine and ecstasy.
How to Stay Safe and Reduce Risks
1. Avoid Drug Use Altogether
The safest option is to avoid using drugs entirely. This might sound simple, but it can be challenging if you or someone you care about struggles with substance use disorder. If that is the case, please know help is available. You do not have to face this alone.
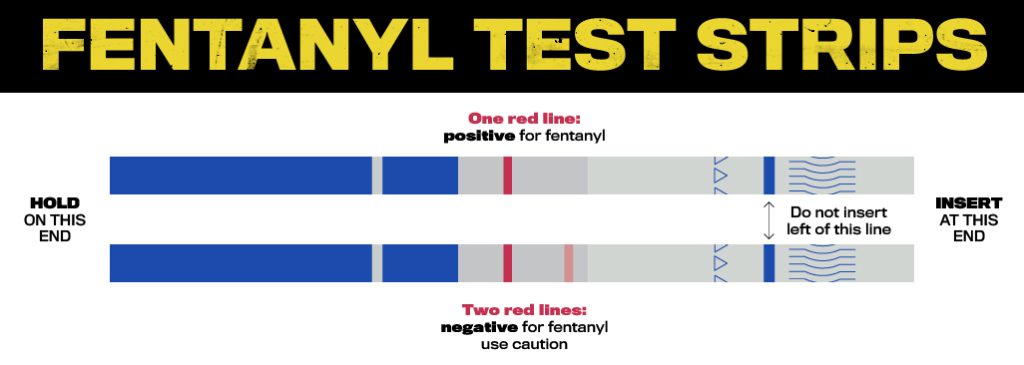
2. Use Fentanyl Test Strips
If you or a loved one does feel at risk of encountering fentanyl, fentanyl test strips can detect whether the drug is present in a powder or a crushed pill. They are not foolproof, but they do lower the risk of an unexpected overdose. Remember, a negative result does not guarantee total safety, so caution is still necessary.
3. Recognize Overdose Signs
An overdose can happen suddenly. If you see someone who has very slow or stopped breathing, is unconscious, or has bluish lips or fingertips, treat that as an emergency and call 911 right away. You should also give naloxone (often known by the brand name Narcan) if it is available. Naloxone reverses opioid overdose by blocking the opioid’s effect on the brain, and it can save a life.

4. Carry Narcan (Naloxone)
Naloxone kits are available at many pharmacies and community organizations. You do not need a prescription in most places. Having a kit on hand can make the difference between life and death if an overdose occurs. Public health agencies often provide Narcan at low or no cost, so you can ask about free programs in your area.
5. Harm Reduction Approaches
Some communities focus on harm reduction to lower the risk of infection, overdose, and other health issues. Harm reduction programs often offer clean syringes, naloxone training, and information about safer use practices. Their goal is to support people who use drugs and to prevent further harm. They also serve as a point of contact for people to enter drug addiction treatment programs or other forms of help.
Mental Health Care and Fentanyl Use
Many people who develop a substance use disorder are also dealing with emotional pain or stress. Mental health care can address underlying issues like anxiety, depression, or unresolved childhood trauma. Counseling or therapy helps you learn healthier ways to cope. You also gain support that can help you move away from drug use.
Remember, you do not have to handle everything on your own. A licensed therapist, psychiatrist, or counselor is there to guide and support you. They help you work on a treatment plan for your needs and challenges. This plan often includes therapy, medication, and group support.

Finding Treatment for Substance Use Disorder
1. Drug Addiction Treatment Programs
Drug addiction treatment programs offer structured help through inpatient or outpatient settings. They often include detox services, counseling, and medication-assisted treatment. These programs give you the tools to stop drug use and maintain long-term health.
2. Support Groups
Groups like Narcotics Anonymous or other community support groups can provide a sense of connection. They let you share experiences with people who understand your challenges. They also offer encouragement to stay on track. Support from peers makes a big difference in your addiction recovery journey.
3. Family Involvement
Family members can play an essential role in recovery. They often notice changes in behavior before anyone else. When a family learns how to support a loved one and set healthy boundaries, it creates a more stable environment for healing. Encourage open, non-judgmental communication. Offer to help with finding resources or simply be there to listen.
If you or someone you care about has a substance use disorder, please remember that help is available. A treatment plan can involve drug addiction treatment programs, therapy, and support groups like Narcotics Anonymous. You also have the option of including family members who want to help. All these resources work together to keep you or your loved one safe and supported.