


Psychedelic-assisted therapy is currently drawing a lot of attention. There has been a resurgence of interest in the therapeutic potential of psychedelic drugs such as psilocybin (found in magic mushrooms), LSD, and MDMA (commonly known as ecstasy) for the treatment of various mental health conditions.
Re-emerging clinical research suggests that psychedelic-assisted therapy has the potential to serve as an alternative treatment for substance use disorder, depression, and anxiety. For example:
There are also numerous stories and testimonies from individuals who have undergone psychedelic-assisted therapy and reported significant improvements in their mental health.
Many of these stories are shared publicly, in the media, or through personal channels, creating a positive and powerful narrative around the potential of psychedelic-assisted therapy. Patients have reported feeling more open, connected, and attuned to their emotions and thoughts and having a deeper understanding of themselves and their place in the world.
All this is very encouraging. However, it's worth noting that we've been here before with psychedelics. In the 1950s and 60s, numerous studies were happening across the United States to explore the potential of psychedelics in treating various mental health conditions.
Media outlets like CBSNews even covered the story of Arthur King, who received LSD as part of his treatment for alcoholism in 1966. After 6 months of treatment with LSD, Arthur King was able to curb his addiction and was still sober in the 27-year follow-up.
But as these drugs became synonymous with substance abuse, hedonism, and countercultural activities, they were made illegal. LSD was made illegal in 1966, followed by mushrooms in 1968, and most research into the therapeutic potential of psychedelics ground to a halt. At the moment, the use of psychedelics for their therapeutic potential is still highly regulated and not yet widely available. But the renewed interest and investment have fueled further research, much of which is ongoing.
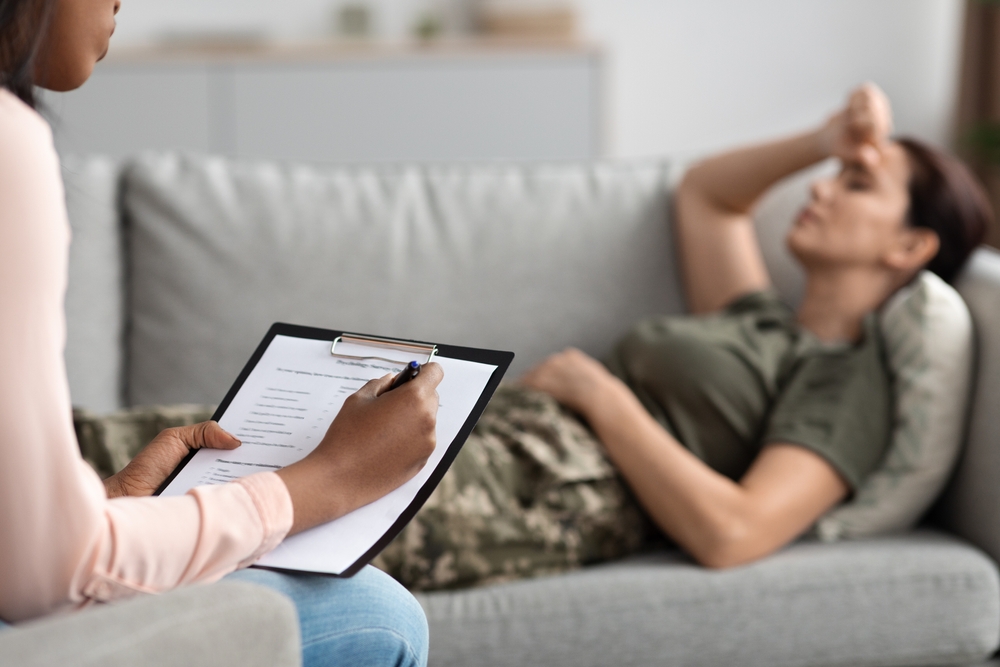
Psychedelic-assisted therapy is a therapeutic approach that uses psychedelic substances, such as psilocybin, Ketamine, and MDMA, to facilitate therapeutic experiences. These substances are administered in a controlled and supportive environment, usually with the guidance of a trained health professional, to help individuals achieve altered states of consciousness that may lead to increased self-awareness, insight, and emotional processing.
The goal of psychedelic-assisted therapy is to provide individuals with a unique and profound experience that allows them to gain new perspectives on their thoughts, feelings, and behaviors and to work through emotional and psychological challenges.
For example, cancer patients who took part in two different studies reported mystical experiences or spiritualistic experiences after taking psilocybin for their anxiety and depression. According to the studies, psilocybin reduced cancer-related anxiety, hopelessness, and dread immediately after the dose, and the improvements persisted for up to 6.5 months in about 80% of the patients.
A growing body of research suggests that psychedelic-assisted treatment may have promise in easing some of the symptoms of addiction. One way psychedelics may help with addiction is by reducing other mental health symptoms that often co-occur, such as depression and anxiety.
For many people struggling with alcohol and opioid addiction, these symptoms can be a significant barrier to recovery, as they can make it harder to stay motivated and engaged in treatment. By addressing these underlying mental health issues, psychedelics may make it easier for individuals to quit abusing substances.
Psychedelic-assisted treatment may also work by promoting changes in brain function and increasing self-awareness. For example, research suggests that psychedelics may help to "reset" the brain by fostering new neural connections and reducing negative thought patterns. By facilitating these changes in the brain, psychedelics may help individuals break free from patterns of addictive behavior and develop healthier coping mechanisms.
Studies have shown that psychedelics reduce both alcohol use and smoking. The success rates are higher than what doctors see with other therapy or medication alone.
While researchers do not fully understand how psychedelics work in the brain, several potential mechanisms have been proposed.

While psychedelic-assisted therapy for addiction treatment may hold promise, there are also potential risks associated with using these substances. They include:
While psychedelics have shown promise as a therapeutic tool, they're not a panacea and don't work for everyone. Factors like dosage, setting, and individual differences in brain chemistry can all impact the effectiveness of psychedelic-assisted therapy. Also, trained professionals should always supervise these substances in a controlled environment, as they can be potentially dangerous if misused.
If you're considering using psychedelics outside of therapy for different reasons, you should seek the support of a Psychedelic harm reduction and integration therapist. A PHRI therapist will help you plan to minimize risks and increase the chances of positive therapeutic outcomes.


